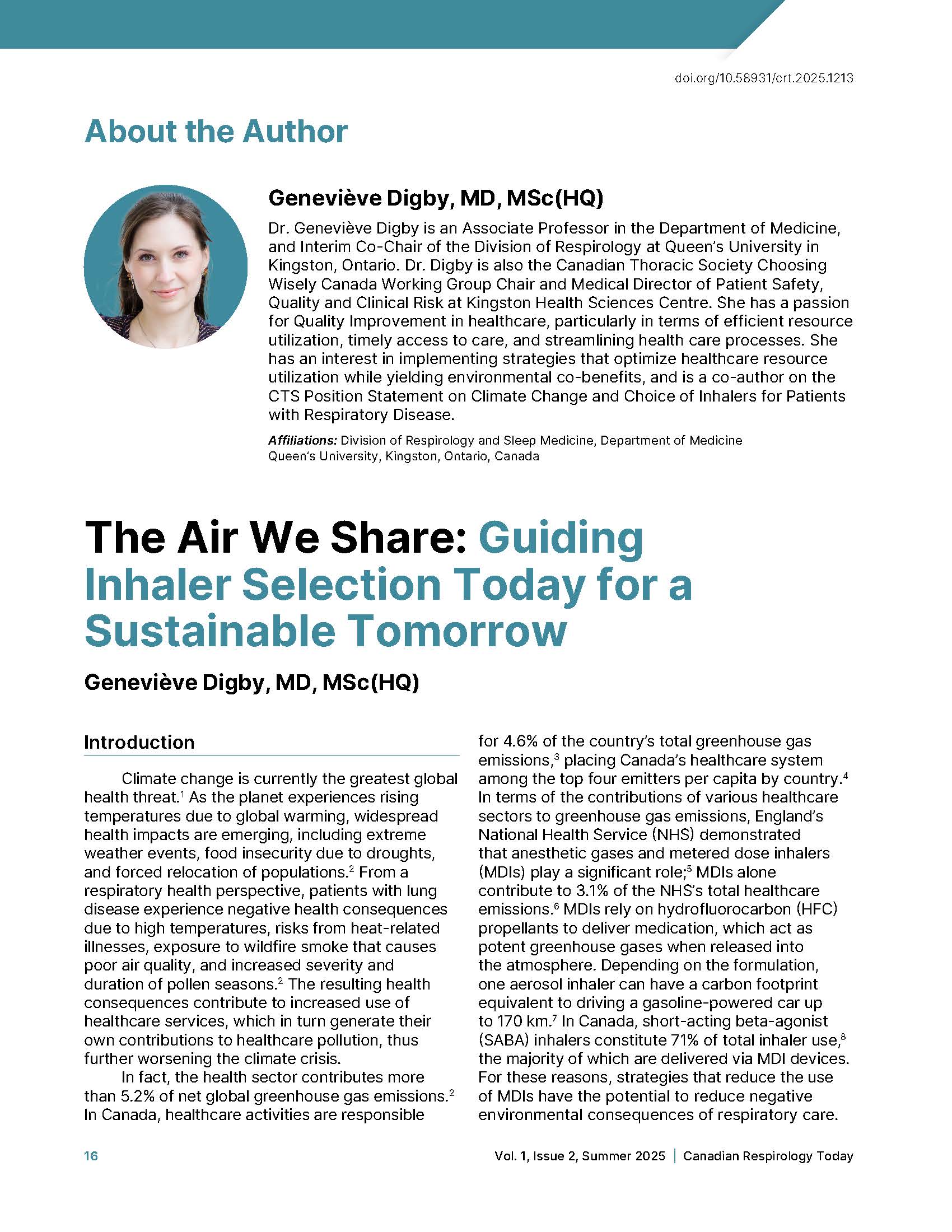
The Air We Share: Guiding Inhaler Selection Today for a Sustainable Tomorrow
DOI:
https://doi.org/10.58931/crt.2025.1213Abstract
Climate change is currently the greatest global health threat. As the planet experiences rising temperatures due to global warming, widespread health impacts are emerging, including extreme weather events, food insecurity due to droughts, and forced relocation of populations. From a respiratory health perspective, patients with lung disease experience negative health consequences due to high temperatures, risks from heat-related illnesses, exposure to wildfire smoke that causes poor air quality, and increased severity and duration of pollen seasons. The resulting health consequences contribute to increased use of healthcare services, which in turn generate their own contributions to healthcare pollution, thus further worsening the climate crisis.
In fact, the health sector contributes more than 5.2% of net global greenhouse gas emissions. In Canada, healthcare activities are responsible for 4.6% of the country’s total greenhouse gas emissions, placing Canada’s healthcare system among the top four emitters per capita by country. In terms of the contributions of various healthcare sectors to greenhouse gas emissions, England’s National Health Service (NHS) demonstrated that anesthetic gases and metered dose inhalers (MDIs) play a significant role; MDIs alone contribute to 3.1% of the NHS’s total healthcare emissions. MDIs rely on hydrofluorocarbon (HFC) propellants to deliver medication, which act as potent greenhouse gases when released into the atmosphere. Depending on the formulation, one aerosol inhaler can have a carbon footprint equivalent to driving a gasoline-powered car up to 170 km. In Canada, short-acting beta-agonist (SABA) inhalers constitute 71% of total inhaler use, the majority of which are delivered via MDI devices. For these reasons, strategies that reduce the use of MDIs have the potential to reduce negative environmental consequences of respiratory care.
References
Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373(9676):1693–1733. doi:10.1016/s0140-6736(09)60935-1
Romanello M, Di Napoli C, Drummond P, Green C, Kennard H, Lampard P, et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet. 2022;400(10363):1619–1654. doi:10.1016/S0140-6736(22)01540-9
Vogel L. Canada’s health system is among the least green. CMAJ. 2019;191(48):E1342-E1343. doi:10.1503/cmaj.1095834
Health care without harm. global road map for health care decarbonization: a navigational tool for achieving zero emissions with climate resilience and health equity: Executive Summary. Health Care Without Harm, 2021. [cited 31 July 2025]. Available from: Global Road Map for Health Care Decarbonization.pdf
Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. The Lancet Planet Health. 2021;5(2):e84–e92. doi:10.1016/S2542-5196(20)30271-0
van Hove M, Leng G. A more sustainable NHS. BMJ. 2019;366:l4930. doi:10.1136/bmj.l4930
CASCADES. Environmentally sustainable opportunities for health systems. Metered dose inhalers (MDIs). 2022. [cited 31 July 2025]. Available from: https://view.publitas.com/5231e51e-4654-42c2-accd-b722e21f3093/metered-dose-inhalers-mdis-infographic/?gl=1*aqoidm*_ga*Njk3NTY4MjE4LjE3MTQ0Nzg0MDc.*_ga_TRM5NF4JFC*MTcxNDQ4ODI0My4yLjEuMTcxNDQ4ODMwNS4wLjAuMA.
Janson C, Maslova E, Wilkinson A, Penz E, Papi A, Budgen N, et al. The carbon footprint of respiratory treatments in Europe and Canada: an observational study from the CARBON programme. Eur Respir J. 2022;60(2):2102760. doi:10.1183/13993003.02760-2021
Sustainable markets initiative. decarbonising patient care pathways. 2022 November. [cited 31 July 2025]. Available from: https://a.storyblok.com/f/109506/x/88fe7ea368/smi-hstf-pcp-whitepaper.pdf.
Gupta S, Couillard S, Digby G, Tse MS, Green S, Aceron R, et al. Canadian Thoracic Society Position Statement on climate change and choice of inhalers for patients with respiratory disease. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine. 2023;7(5):232–239. https://doi.org/10.1080/24745332.2023.2254283
Green S, Stoynova V, Culley C, Kaplan A, Hale I, Simms N, et al. Climate-conscious inhaler prescribing for family physicians. Can Fam Physician. 2024;70(6):381–387. doi:10.46747/cfp.7006381
Diab N, Gershon AS, Sin DD, Tan WC, Bourbeau J, Boulet LP, et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–1139. doi:10.1164/rccm.201804-0621CI
Aaron SD, Vandemheen KL, FitzGerald JM, Ainslie M, Gupta S, Lemière C, et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA. 2017;317(3):269–279. doi:10.1001/jama.2016.19627
Gupta S, Goodridge D, Pakhale S, McIntyre K, Pendharkar SR. Choosing wisely: the Canadian Thoracic Society’s list of six things that physicians and patients should question. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine. 2017;1(2):54–61. doi:10.1080/24745332.2017.1331666
Pavord ID, Mathieson N, Scowcroft A, Pedersini R, Isherwood G, Price D. The impact of poor asthma control among asthma patients treated with inhaled corticosteroids plus long-acting β(2)-agonists in the United Kingdom: a cross-sectional analysis. NPJ Prim Care Respir Med. 2017;27(1):17. doi:10.1038/s41533-017-0014-1
Tsao CL, Chan SY, Lee MH, Hsieh TYJ, Phipatanakul W, Ruran HB, et al. Adverse outcomes associated with short-acting beta-agonist overuse in asthma: a systematic review and meta-analysis. Allergy. 2025;80(6):1629–1646. doi:10.1111/all.16538
Wilkinson AJK, Maslova E, Janson C, Radhakrishnan V, Quint JK, Budgen N, et al. Greenhouse gas emissions associated with suboptimal asthma care in the UK: the SABINA healthCARe-Based envirONmental cost of treatment (Confalonieri, #71) study. Thorax. 2024;79(5):412–421. doi:10.1136/thorax-2023-220259
Global Initiative for Asthma (Gussoni, #141). Global strategy for asthma management and prevention, 2024. [updated May 2024, cited 31 July 2025]. Available from: https://ginasthma.org/wp-content/uploads/2024/05/GINA-2024-Strategy-Report-24_05_22_WMS.pdf.
Hatter L, Holliday M, Eathorne A, Bruce P, Pavord ID, Reddel HK, et al. The carbon footprint of as-needed budesonide/formoterol in mild asthma: a post hoc analysis. Eur Respir J. 2024;64(1):2301705. doi:10.1183/13993003.01705-2023
Bell J, Graul E, Nordon C, Kallis C, Whittaker HR, Janson C, et al. EXACOS CARBON: describing the greenhouse gas emissions of healthcare resource utilization by frequency and severity of COPD exacerbation in England [abstract]. Am J Respir Crit Care Med. 2024;209:A2113. https://doi.org/10.1164/ajrccm-conference.2024.209.1_MeetingAbstracts.A2113
Bourbeau J, Bhutani M, Hernandez P, Aaron SD, Beauchesne M-F, Kermelly SB, et al. 2023 Canadian Thoracic Society Guideline on Pharmacotherapy in Patients with Stable COPD. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine. 2023;7(4):173–191. https://doi.org/10.1080/24745332.2023.2231451
Global Initiative for Chronic Obstructive Lung Disease. 2025 GOLD Report. Global Strategy for Prevention, Diagnosis and Management of COPD 2025 Report. 2025. [cited 31 July 2025]. Available from: https://goldcopd.org/2025-gold-report/
Panigone S, Sandri F, Ferri R, Volpato A, Nudo E, Nicolini G. Environmental impact of inhalers for respiratory diseases: decreasing the carbon footprint while preserving patient-tailored treatment. BMJ Open Respir Res. 2020;7(1):e000571. doi:10.1136/bmjresp-2020-000571
Welch MJ, Nelson HS, Shapiro G, Bensch GW, Sokol WN, Smith JA, et al. Comparison of patient preference and ease of teaching inhaler technique for Pulmicort Turbuhaler® versus pressurized metered-dose inhalers. J Aerosol Med. 2004;17(2):129–139. doi:10.1089/0894268041457174
Gálffy G, Szilasi M, Tamási L. P227 Clinical effectiveness, health-related quality of life and patient satisfaction after switch from metered dose inhaler to easyhaler dry powder inhaler in patients with asthma and COPD; a real-life study. Thorax. 2019;74(Suppl 2):A212–A213. doi:10.1136/thorax-2019-BTSabstracts2019.370
Wilkinson AJK, Braggins R, Steinbach I, Smith J. Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England. BMJ Open. 2019;9(10):e028763. doi:10.1136/bmjopen-2018-028763
Al-Jahdali H, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Bin Salih S, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol. 2013;9(1):8. doi:10.1186/1710-1492-9-8
Volerman A, Delesha C, Press V. What can be done to impact respiratory inhaler misuse: exploring the problem, reasons, and solutions. Expert Rev Respir Med. 2020;14(8):791–805. doi:10.1080/17476348.2020.1754800
Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol. 2007;119(6):1537–1538. doi:10.1016/j.jaci.2007.02.037
Murphy AC, Carroll W, Gotsell M, Potter C, Quint JK, Malone R. How do patients determine when their inhaler is empty? Insights from an analysis of returned inhalers and a patient survey. BMJ Open Respir Res. 2024;11(1):e002579. doi:10.1136/bmjresp-2024-002579
Quantz D, Wong GYC, Liang K. Patient perspectives on the environmental impact of inhalers: a survey in British Columbia. Can Pharm J (Ott). 2023;156(6):298–302. doi:10.1177/17151635231202980
Go Zero. Informational leaflet. Recycling process material treatment. [cited 31 July 2025]. Available from: https://cdn.shopify.com/s/files/1/0529/3342/7365/files/230907_Information-leaflet_EN.pdf?v=1700842499
Hargreaves C, Budgen N, Whiting A, Lachacz K, Sommerville M, Archbell J, et al. S60 A new medical propellant HFO-1234ze(E): reducing the environmental impact of inhaled medicines. Thorax. 2022;77(Suppl 1):A38–A39. doi:10.1136/thorax-2022-BTSabstracts.66