Antifibrotics in Non-Idiopathic Pulmonary Fibrosis Interstitial Lung Diseases
DOI:
https://doi.org/10.58931/crt.2025.1318Abstract
Case 1
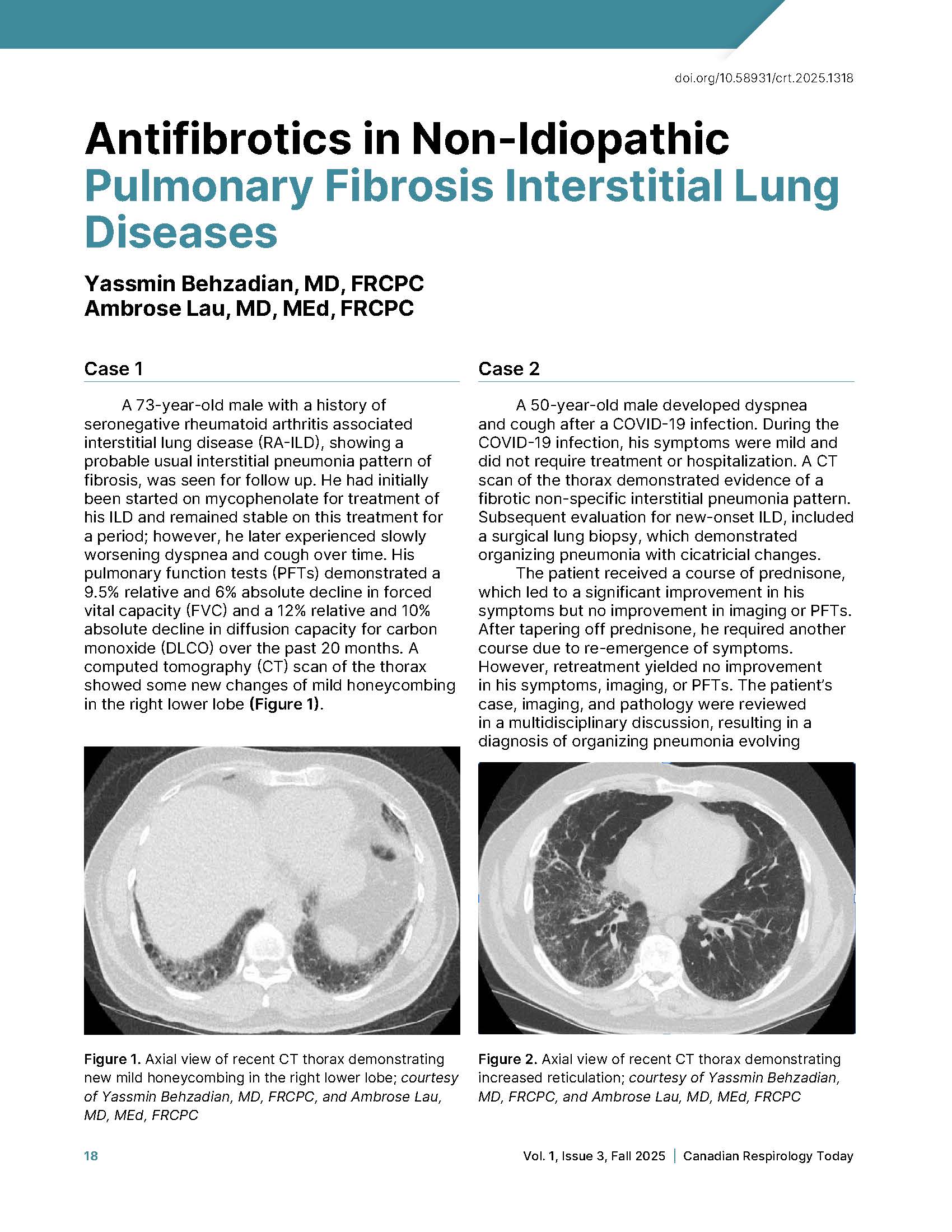
A 73-year-old male with a history of seronegative rheumatoid arthritis associated interstitial lung disease (RA-ILD), showing a probable usual interstitial pneumonia pattern of fibrosis, was seen for follow up. He had initially been started on mycophenolate for treatment of his ILD and remained stable on this treatment for a period; however, he later experienced slowly worsening dyspnea and cough over time. His pulmonary function tests (PFTs) demonstrated a 9.5% relative and 6% absolute decline in forced vital capacity (FVC) and a 12% relative and 10% absolute decline in diffusion capacity for carbon monoxide (DLCO) over the past 20 months. A computed tomography (CT) scan of the thorax showed some new changes of mild honeycombing in the right lower lobe (Figure 1).
Case 2
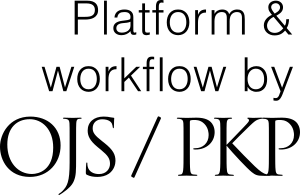
A 50-year-old male developed dyspnea and cough after a COVID-19 infection. During the COVID-19 infection, his symptoms were mild and did not require treatment or hospitalization. A CT scan of the thorax demonstrated evidence of a fibrotic non-specific interstitial pneumonia pattern. Subsequent evaluation for new-onset ILD, included a surgical lung biopsy, which demonstrated organizing pneumonia with cicatricial changes.
The patient received a course of prednisone, which led to a significant improvement in his symptoms but no improvement in imaging or PFTs. After tapering off prednisone, he required another course due to re-emergence of symptoms. However, retreatment yielded no improvement in his symptoms, imaging, or PFTs. The patient’s case, imaging, and pathology were reviewed in a multidisciplinary discussion, resulting in a diagnosis of organizing pneumonia evolving toward a more fibrotic phenotype. In addition to his worsening symptoms, imaging revealed increased reticulation, and assessments showed a significant decline in his FVC and DLCO over time.
References
Raghu G, Remy-Jardin M, Richeldi L, Thomson CC, Inoue Y, Johkoh T, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am J Respir Crit Care Med. 2022;205(9):e18-e47. doi:10.1164/rccm.202202-0399ST
Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SLF, Inoue Y, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med. 2019;381(18):1718-1727. doi:10.1056/NEJMoa1908681
Jang JH, Choe EJ, Jung SY, Ko J, Kim DW, Lee JH. A study on the prevalence and prognosis of progressive pulmonary fibrosis: a retrospective observational study. Medicine (Baltimore). 2024;103(20):e38226. doi:10.1097/MD.0000000000038226
Brown KK, Martinez FJ, Walsh SLF, Thannickal VJ, Prasse A, Schlenker-Herceg R, et al. The natural history of progressive fibrosing interstitial lung diseases. Eur Respir J. 2020;55(6):2000085. Published 2020 Jun 25. doi:10.1183/13993003.00085-2020
Wollin L, Wex E, Pautsch A, Schnapp G, Hostettler KE, Stowasser S, et al. Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur Respir J. 2015;45(5):1434-1445. doi:10.1183/09031936.00174914
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071-2082. doi:10.1056/NEJMoa1402584
Distler O, Highland KB, Gahlemann M, Azuma A, Fischer A, Mayes MD, et al. Nintedanib for systemic sclerosis–associated interstitial lung disease. N Engl J Med. 2019;380(26):2518-2528. doi:10.1056/NEJMoa1903076
Highland KB, Distler O, Kuwana M, Allanore Y, Assassi S, Azuma, A, et al. Efficacy and safety of nintedanib in patients with systemic sclerosis-associated interstitial lung disease treated with mycophenolate: a subgroup analysis of the SENSCIS trial. Lancet Respir Med. 2021;9(1):96-106. doi:10.1016/S2213-2600(20)30330-1
Wells AU, Flaherty KR, Brown KK, Inoue Y, Devaraj A, Richeldi L, et al. Nintedanib in patients with progressive fibrosing interstitial lung diseases—subgroup analyses by interstitial lung disease diagnosis in the INBUILD trial: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Respir Med. 2020;8(5):453-460. doi:10.1016/S2213-2600(20)30036-9
King TE, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083-2092. doi:10.1056/NEJMoa1402582
Behr J, Prasse A, Kreuter M, Johow J, Rabe KF, Bonella, F, et al. Pirfenidone in patients with progressive fibrotic interstitial lung diseases other than idiopathic pulmonary fibrosis (RELIEF): a double-blind, randomised, placebo-controlled, phase 2b trial. Lancet Respir Med. 2021;9(5):476-486. doi:10.1016/S2213-2600(20)30554-3
Solomon JJ, Danoff SK, Woodhead FA, Hurwitz S, Maurer R, Glaspole I, et al. Safety, tolerability, and efficacy of pirfenidone in patients with rheumatoid arthritis-associated interstitial lung disease: a randomised, double-blind, placebo-controlled, phase 2 study. Lancet Respir Med. 2023;11(1):87-96. doi:10.1016/S2213-2600(22)00260-0
Richeldi L. Azuma A, Cottin V, Kreuter M, Maher TM, Martinez FJ, et al. Nerandomilast in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2025;392(22):2193-2202. doi:10.1056/NEJMoa2414108
Maher TM, Assassi S, Azuma A, Cottin V, Hoffmann-Vold A-M, Kreuter M, et al. Nerandomilast in patients with progressive pulmonary fibrosis. N Engl J Med. 2025;392(22):2203-2214. doi:10.1056/NEJMoa2503643
Johnson SR, Bernstein EJ, Bolster MB, Chung JH, Danoff SK, George MD, et al. 2023 American College of Rheumatology (ACR)/American College of Chest Physicians (CHEST) Guideline for the treatment of interstitial lung disease in people with systemic autoimmune rheumatic diseases. Arthritis Rheumatol. 2024;76(8):1182-1200. doi:10.1002/art.42861