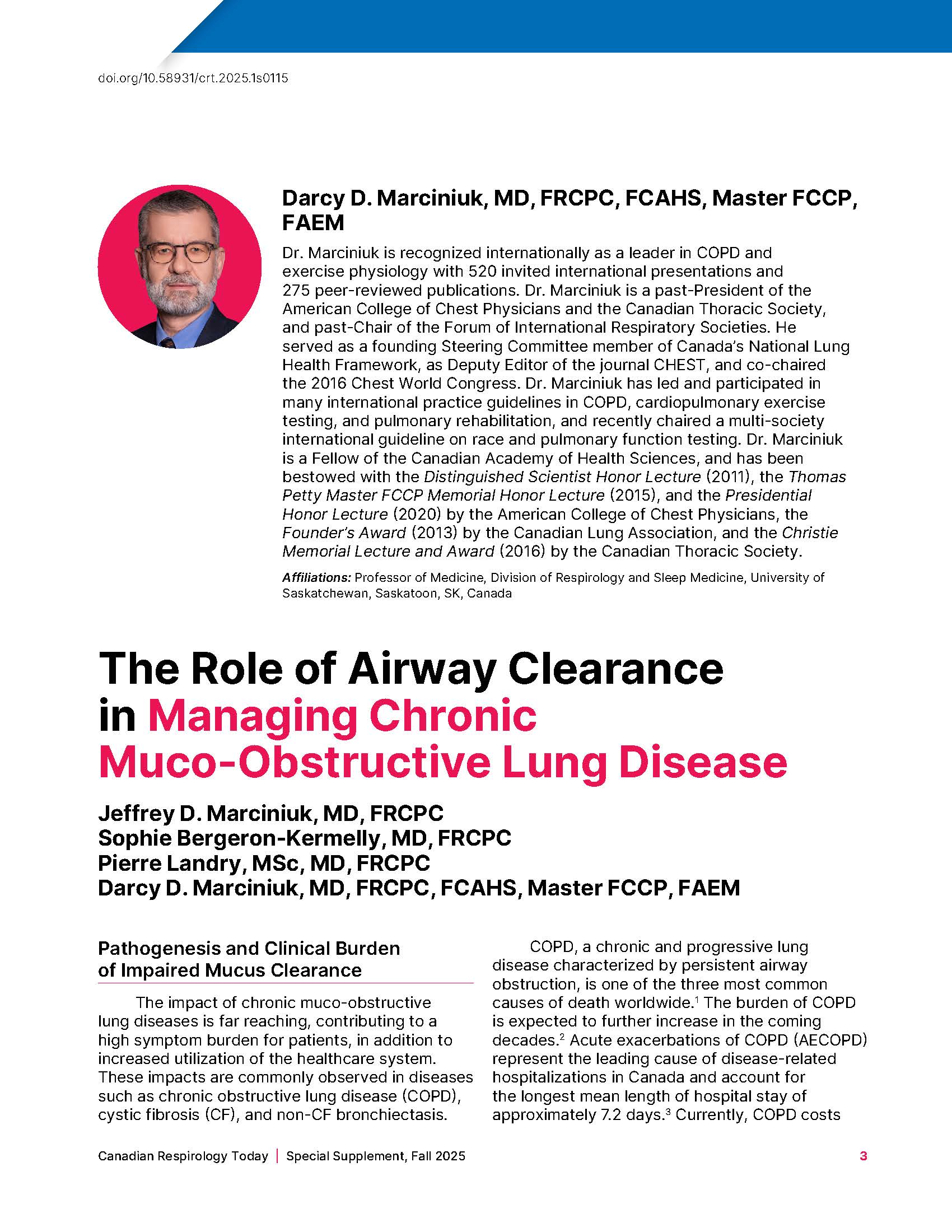
The Role of Airway Clearance in Managing Chronic Muco‑Obstructive Lung Disease
DOI:
https://doi.org/10.58931/crt.2025.1s0115Abstract
The impact of chronic muco-obstructive lung diseases is far reaching, contributing to a high symptom burden for patients, in addition to increased utilization of the healthcare system. These impacts are commonly observed in diseases such as chronic obstructive lung disease (COPD), cystic fibrosis (CF), and non-CF bronchiectasis.
COPD, a chronic and progressive lung disease characterized by persistent airway obstruction, is one of the three most common causes of death worldwide. The burden of COPD is expected to further increase in the coming decades. Acute exacerbations of COPD (AECOPD) represent the leading cause of disease‑related hospitalizations in Canada and account for the longest mean length of hospital stay of approximately 7.2 days. Currently, COPD costs the Canadian healthcare system, in Canadian dollars, $1.5 billion annually, and is expected to exceed $9.0 billion by 2030. Chronic Bronchitis (CB), a very common condition in patients with COPD, is classically defined as a chronic productive cough lasting at least three months per year for two consecutive years.
References
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi:10.1371/journal.pmed.0030442
Canadian Institute for Health Information. Inpatient hospitalization, surgery, newborn, alternate level of care and childbirth statistics, 2017–2018 [Internet]. April 2019. [cited 2025 Nov 11]. Available from: https://www.cihi.ca/sites/default/files/document/dad-hmdb-childbirth-quick-stats-2017-2018-snapshot-en-web.pdf
Canadian Institute for Health Information. COPD: a focus on high users — Infographic [Internet]. [cited 2025 Nov 11]. Available from: https://www.cihi.ca/en/copd-a-focus-on-high-users-infographic
Risebrough NA, Mursleen S, Ndirangu K, Shah D, Martin A, Schroeder M, et al. The long-term clinical and economic benefits of treating advanced COPD patients with single-inhaler triple therapy in Quebec, Canada - The IMPACT trial. Respir Med. 2024;231:107694. doi:10.1016/j.rmed.2024.107694
Cystic Fibrosis Canada. Canada’s cystic fibrosis population continues to grow, even as some face severe complications [Internet]. 21 Mar 2025. [cited 11 Nov 2025]. Available from: https://cysticfibrosis.ca/news/canadas-cystic-fibrosis-population-continues-to-grow
Jose RJ, Loebinger MR. Clinical and radiological phenotypes and endotypes. Semin Respir Crit Care Med. 2021;42(4):549–555. doi:10.1055/s-0041-1730894
Fahy JV, Dickey BF. Airway mucus function and dysfunction. N Engl J Med. 2010;363(23):2233–2247. doi:10.1056/NEJMra0910061
Thornton DJ, Sheehan JK. From mucins to mucus: toward a more coherent understanding of this essential barrier. Proc Am Thorac Soc. 2004;1(1):54–61. doi:10.1513/pats.2306016
Rubin BK. Mucus and mucins. Otolaryngol Clin North Am. 2010;43(1):27–34, vii–viii. doi:10.1016/j.otc.2009.11.002
Hogg JC. Pathophysiology of airflow limitation in chronic obstructive pulmonary disease. Lancet. 2004;364(9435):709–721. doi:10.1016/S0140-6736(04)16900-6
Kesimer M, Ford AA, Ceppe A, Radicioni G, Cao R, Davis CW, et al. Airway mucin concentration as a marker of chronic bronchitis. N Engl J Med. 2017;377(10):911–922. doi:10.1056/NEJMoa1701632
Hughes GW, Ridley C, Collins R, Roseman A, Ford R, Thornton DJ. The MUC5B mucin polymer is dominated by repeating structural motifs and its topology is regulated by calcium and pH. Sci Rep. 2019;9(1):17350. Published 2019 Nov 22. doi:10.1038/s41598-019-53768-0
Global Institute for Chronic Obstructive Lung Disease. 2024 GOLD report. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease – 2024 report [Internet]. [cited 11 Nov 2025]. Available from: https://goldcopd.org/2024-gold-report/
Bosse Y, Riesenfeld EP, Pare PD, Irvin CG. It’s not all smooth muscle: non-smooth-muscle elements in control of resistance to airflow. Annu Rev Physiol. 2010;72:437–462. doi:10.1146/annurev-physiol-021909-135851
Dunican EM, Elicker BM, Henry T, Gierada DS, Schiebler ML, Anderson W, et al. Mucus plugs and emphysema in the pathophysiology of airflow obstruction and hypoxemia in smokers. Am J Respir Crit Care Med. 2021;203(8):957–968. doi:10.1164/rccm.202006-2248OC
Bourbeau J, Bhutani M, Hernandez P, Aaron SD, Beauchesne MF, Kermelly SB, et al. 2023 Canadian Thoracic Society Guideline on pharmacotherapy in patients with stable COPD. Can J Resp Crit Care Sleep Med 2023. 2023;7:173–191. doi:10.1080/24745332.2023.2231451
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. doi:10.1164/rccm.201309-1634ST
Marciniuk DD, Brooks D, Butcher S, Debigare R, Dechman G, Ford G, et al. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease--practical issues: a Canadian Thoracic Society Clinical Practice Guideline. Can Respir J. 2010;17(4):159–168. doi:10.1155/2010/425975
Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA, et al. Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest. 2007;131(5 Suppl):4S–42S. doi:10.1378/chest.06-2418
O’Donnell DE, Aaron S, Bourbeau J, Hernandez P, Marciniuk DD, Balter M, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease - 2007 update. Can Respir J. 2007;14 Suppl B(Suppl B):5B–32B. doi:10.1155/2007/830570
Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173(12):1390–1413. doi:10.1164/rccm.200508-1211ST
Canadian Agency for Drugs and Technologies in Health (CADTH). Pulmonary rehabilitation for chronic obstructive pulmonary disease: clinical, economic, and budget impact analysis. CADTH Technol Overv. 2010;1(4):e0127.
Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P, et al. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015;147(4):894–942. doi:10.1378/chest.14-1676
Lindenauer PK, Stefan MS, Pekow PS, Mazor KM, Priya A, Spitzer KA, et al. Association between initiation of pulmonary rehabilitation after hospitalization for COPD and 1-Year survival among medicare beneficiaries. JAMA. 2020;323(18):1813–1823. doi:10.1001/jama.2020.4437
Camp PG, Hernandez P, Bourbeau J, Kirkham A, Debigare R, Stickland MK, et al. Pulmonary rehabilitation in Canada: a report from the Canadian Thoracic Society COPD Clinical Assembly. Can Respir J. 2015;22(3):147–152. doi:10.1155/2015/369851
Southern KW, Addy C, Bell SC, Bevan A, Borawska U, Brown C, et al. Standards for the care of people with cystic fibrosis; establishing and maintaining health. J Cyst Fibros. 2024;23(1):12–28. doi:10.1016/j.jcf.2023.12.002
Hill AT, Sullivan AL, Chalmers JD, De Soyza A, Elborn SJ, Floto AR, et al. British Thoracic Society Guideline for bronchiectasis in adults. Thorax. 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
McIlwaine MP, Alarie N, Davidson GF, Lands LC, Ratjen F, Milner R, et al. Long-term multicentre randomised controlled study of high frequency chest wall oscillation versus positive expiratory pressure mask in cystic fibrosis. Thorax. 2013;68(8):746–751. doi:10.1136/thoraxjnl-2012-202915
Cystic Fibrosis Trust, Physiotherapy Working Group members. Morrison L, Parrott H, editors. Standards of Care and Good Clinical Practice for the Physiotherapy Management of Cystic Fibrosis fourth edition [Internet]. London, UK: Cystic Fibrosis Trust December 2020. [cited 11 Nov 2025]. Available from: https://www.cysticfibrosis.org.uk/sites/default/files/2020-12/Standards%20of%20Care%20and%20Good%20Clinical%20Practice%20for%20the%20Physiotherapy%20Management%20of%20Cystic%20Fibrosis%20Fourth%20edition%20December%202020.pdf
Trudell Medical International. Aerobika oscillating positive expiratory pressure device - study summary. January 2024. [cited 11 Nov 2025]. Available from: https://www.trudellmed.com/sites/default/files/documents/aerobika-opep-study-summary-2024.pdf
Alghamdi SM, Alsulayyim AS, Alasmari AM, Philip KEJ, Buttery SC, Banya WAS, et al. Oscillatory positive expiratory pressure therapy in COPD (O-COPD): a randomised controlled trial. Thorax. 2023;78(2):136–143. doi:10.1136/thorax-2022-219077
Lee AL, Williamson HC, Lorensini S, Spencer LM. The effects of oscillating positive expiratory pressure therapy in adults with stable non-cystic fibrosis bronchiectasis: a systematic review. Chron Respir Dis. 2015;12(1):36–46. doi:10.1177/1479972314562407
Morrison L, Milroy S. Oscillating devices for airway clearance in people with cystic fibrosis. Cochrane Database Syst Rev. 2020;4(4):CD006842. Published 2020 Apr 30. doi:10.1002/14651858.CD006842.pub5
Thanh NX, Jacobs P, Suggett J, McIvor A, Kaplan A. Cost-effectiveness of the Aerobika® oscillating positive expiratory pressure device in the management of chronic obstructive pulmonary disease exacerbations in Canada. Can Respir J. 2019;2019:9176504. Published 2019 Jan 10. doi:10.1155/2019/9176504
Khoudigian-Sinani S, Kowal S, Suggett JA, Coppolo DP. Cost-effectiveness of the Aerobika* oscillating positive expiratory pressure device in the management of COPD exacerbations. Int J Chron Obstruct Pulmon Dis. 2017;12:3065–3073. Published 2017 Oct 19. doi:10.2147/COPD.S143334
Burudpakdee C, Seetasith A, Dunne P, Kauffman G, Carlin B, Coppolo Det al. A real-world study of 30-day exacerbation outcomes in chronic obstructive pulmonary disease (COPD) patients managed with Aerobika OPEP. Pulm Ther. 2017;3:163–171. doi: https://doi.org/10.1007/s41030-017-0027-5
Svenningsen S, Paulin GA, Sheikh K, Guo F, Hasany A, Kirby M, et al. Oscillatory positive expiratory pressure in chronic obstructive pulmonary disease. COPD. 2016;13(1):66–74. doi:10.3109/15412555.2015.1043523
Kim SR, Kim SH, Kim GH, Cho JY, Choi H, Lee H, et al. Effectiveness of the use of an oscillating positive expiratory pressure device in bronchiectasis with frequent exacerbations: a single-arm pilot study. Front Med (Lausanne). 2023;10:1159227. Published 2023 May 12. doi:10.3389/fmed.2023.1159227
Tse J, Wada K, Wang Y, Coppolo D, Kushnarev V, Suggett J. Impact of oscillating positive expiratory pressure device use on post-discharge hospitalizations: a retrospective cohort study comparing patients with COPD or chronic bronchitis using the Aerobika® and Acapella® devices. Int J Chron Obstruct Pulmon Dis. 2020;15:2527–2538. Published 2020 Oct 19. doi:10.2147/COPD.S256866